Liquid Cytology
Liquid-based cytology is a method of preparing samples for examination in cytopathology. The sample is collected, normally by a small brush, in the same way as for a conventional smear test, but rather than the smear being transferred directly to a microscope slide, the sample is deposited into a small bottle of preservative liquid.
Cytopathology, a branch of pathology, deals with manifestations of disease at the cellular level. Liquid-based cytology is a method of preparing samples for examination in cytopathology.
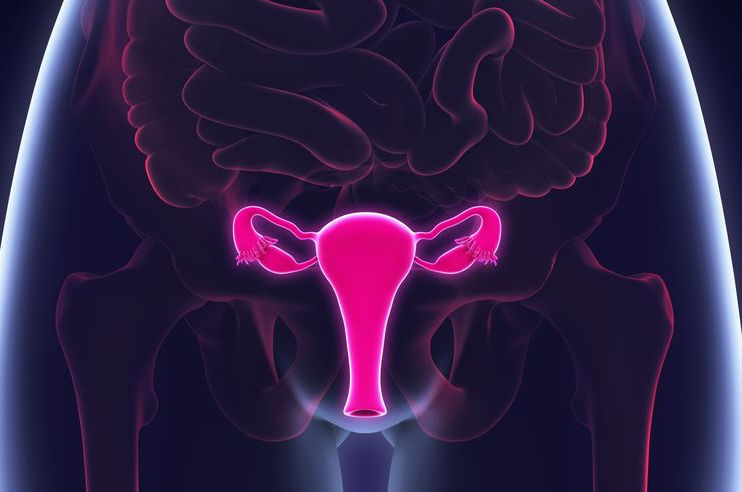
Liquid-based cytology is an alternative to the Pap test (smear test). Both form part of a cervical cancer screening that can also include an HPV test and physical pelvis examination. The goal of a cervical screening is to check for abnormal cervical cells that could be precancerous/cancerous and diagnose abnormal cells and provide treatment if necessary. Regular (as required) screening helps reduce the incidence of cervical cancer and mortality.
What Happens During Liquid-based Cytology
Like a Pap smear, Liquid-based Cytology (LBC) involves collecting (‘scraping’) a sample of cells from the surface of the cervix.
A small brush is used to collect the cells (a spatula in the case of a Pap smear). Cells from LBC remain on the head of the brush which gets broken off and placed into a small pot of liquid that goes to a lab. Cells collected during a Pap smear are transferred to a microscope slide and sent to a lab. Once at a lab, a careful examination takes place. Once complete, results are communicated to the healthcare professional who then informs the patient. Results fall into the following categories:
Normal: No cell changes observed.
Unclear: Cells might be abnormal. Significant changes could not be confirmed which could be a sign of precancer. Abnormal cells could be connected to HPV, infection, pregnancy or life changes. A follow-up test should be recommended.
Abnormal: Abnormal cells do not necessarily equal cancer. More testing is needed to see whether it is, or is becoming, cancer. ‘Low-grade’ changes are usually minor while ‘high-grade’ changes are considered (more) serious.
Not all HPV strains lead to cervical (and other) cancer, however, HPV is found in 99% of cervical cancers making it the main cause of cervical cancer.
Precancer needs to be addressed. Early diagnosis helps to simplify treatment and improve outcome. When a patient has pre-cancerous cells it does not mean she has cervical cancer.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Phasellus ac aliquam velit. Phasellus dapibus cursus erat, quis consequat urna efficitur non. Phasellus cursus, erat quis mollis lobortis, urna risus hendrerit metus, id dictum metus purus vel magna. Nulla non purus sit amet arcu convallis egestas
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Phasellus ac aliquam velit. Phasellus dapibus cursus erat, quis consequat urna efficitur non. Phasellus cursus, erat quis mollis lobortis, urna risus hendrerit metus, id dictum metus purus vel magna. Nulla non purus sit amet arcu convallis egestas
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Phasellus ac aliquam velit. Phasellus dapibus cursus erat, quis consequat urna efficitur non. Phasellus cursus, erat quis mollis lobortis, urna risus hendrerit metus, id dictum metus purus vel magna. Nulla non purus sit amet arcu convallis egestas

COSMETIC SURGERY
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.

COSMETIC SURGERY
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.

COSMETIC SURGERY
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
